Birth control choices shape our lives, yet we often overlook their long-term impact. The Paragard IUD, a hormone-free option, has gained popularity among those seeking a set-it-and-forget-it approach.
According to the Cleveland Clinic, intrauterine devices (IUDs) are the preferred method of reversible birth control for approximately 23% of women worldwide. But is it truly a worry-free solution?
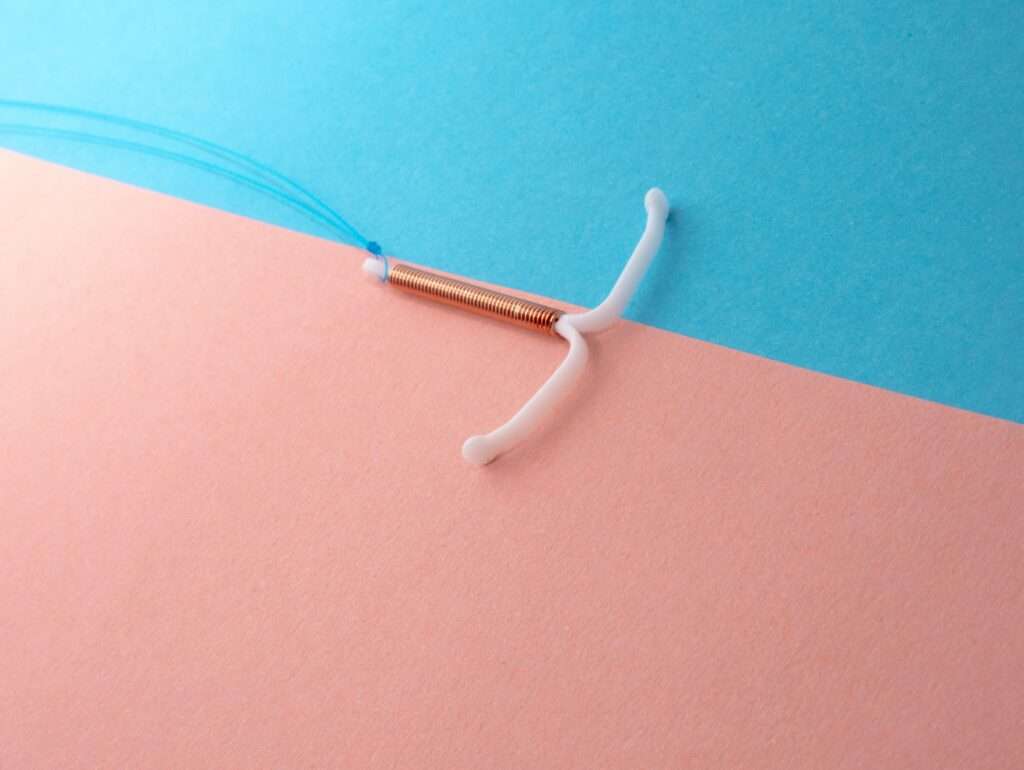
While Paragard boasts impressive efficacy rates, it’s not without risks. As with any medical device, complications can arise, ranging from minor discomfort to serious health concerns. Understanding these potential issues isn’t about fear-mongering—it’s about empowerment.
Knowledge is your best defense for safeguarding your reproductive health. By familiarizing yourself with possible complications, you’re better equipped to make informed decisions and spot warning signs early.
Let’s delve into the world of Paragard, exploring its intricacies and uncovering the hidden challenges that users might face. Are you ready to take control of your contraceptive journey?
Uterine Perforation
Uterine perforation is a rare but serious Paragard complication, where the IUD penetrates the uterine wall. According to the National Institutes of Health, its overall occurrence rate is around 0.2% after 1 year and 0.6% after 5 years. Furthermore, the general likelihood of IUD expulsion is approximately 5% over 5 years.
Risk factors amplify this danger. Uterine anomalies, like bicornuate or septate uteri, increase perforation risk due to atypical anatomy. According to Drugwatch, immediate postpartum insertion, when the uterus is still involuting, elevates the likelihood of this complication sevenfold.
Additionally, the risk of perforation increases by approximately one-third when the device is inserted during lactation.
Early recognition is crucial. Patients may experience severe, localized pelvic pain that worsens with movement. Abnormal bleeding patterns, often heavier than usual menstruation, can also signal perforation. In some cases, missing IUD strings during self-checks may indicate a problem.
Diagnosis relies on imaging. Transvaginal ultrasound is the first-line tool, offering real-time visualization of the uterus and IUD position. If the results are inconclusive, X-rays can help locate a displaced device. In complex cases, CT scans provide detailed 3D imaging, aiding in surgical planning if removal is necessary.
Swift identification and intervention are paramount to prevent further complications and preserve fertility.
Pelvic Inflammatory Disorder
Pelvic inflammatory disease (PID) is an infectious and inflammatory condition that affects the upper female reproductive system. As Medscape states, at risk are the uterus, fallopian tubes, and other pelvic structures. In serious cases, abdominal infection and inflammation can extend to the perihepatic tissues.
More than one million women get diagnosed with this disorder every year in the US. Now, for Paragard users, it’s crucial to understand its pathophysiology. The copper IUD’s presence can potentially disrupt the cervical mucus barrier, allowing pathogens to ascend.
The temporal relationship between insertion and PID risk is noteworthy. According to the Centers for Disease Control and Prevention, the risk of PID from IUDs exists for the first 20 days post-insertion. This underscores the importance of aseptic technique during placement.
Clinically, PID manifests as a triad: pelvic pain, fever, and abnormal discharge. However, presentations can be subtle. Atypical symptoms may include dyspareunia or menstrual irregularities.
Diagnostically, elevated inflammatory markers like C-reactive protein and erythrocyte sedimentation rate are common. Imaging plays a pivotal role; transvaginal ultrasound may reveal thickened, fluid-filled fallopian tubes. In equivocal cases, MRI can delineate tubo-ovarian abscesses.
Recognizing PID early is paramount. Prompt intervention mitigates long-term sequelae, including infertility and chronic pelvic pain.
According to TorHoerman Law, if you have experienced such complications from IUD usage, you can file a lawsuit against the manufacturers. You can sue Cooper Surgical and Teva Pharmaceuticals for their alleged involvement in unfair marketing practices.
These pharmaceutical companies can be held accountable for downplaying the serious dangers associated with their IUDs.
The extent of the damages you have incurred correlates with the amount of compensation you might receive. Regarding prospective Paragard lawsuit settlement amounts, it is projected that each client could get a sum ranging from $10,000 to $400,000.
However, these estimates rely on previous outcomes in comparable legal cases and do not ensure financial recompense for Paragard lawsuits.
Ectopic Pregnancy
The Paragard IUD’s contraceptive efficacy is remarkable, with a failure rate below 1% in the first year post-insertion. However, this high efficacy paradoxically amplifies the risk of ectopic pregnancy in the rare event of conception.
Ectopic gestation, a perilous complication, involves implantation in the fallopian tubes. This abnormal implantation site can lead to tubal rupture if left undiagnosed.
Red flags include unilateral pelvic pain, often described as sharp or cramping, and vaginal spotting. Shoulder pain may signal diaphragmatic irritation from internal bleeding.
Untreated ectopic pregnancies can be catastrophic. Tubal damage is a common outcome, which may compromise future fertility. In severe cases, massive intraperitoneal hemorrhage can occur, posing a significant threat to maternal life.
Timely identification and intervention are crucial in mitigating these risks. Healthcare providers must maintain a high index of suspicion for ectopic pregnancy in Paragard users presenting with suggestive symptoms.
Device Migration
Paragard IUD displacement presents a significant clinical concern. The device may shift from its optimal uterine position, potentially rotating or embedding in the myometrium. This phenomenon can occur at any point post-insertion, often triggered by uterine contractions or pelvic trauma.
Symptoms of migration include dysmenorrhea, menorrhagia, and dyspareunia. Physical indicators comprise shortened or absent retrieval strings and impalpable devices during self-examination.
Diagnostic imaging, such as transvaginal ultrasound or pelvic radiography, is crucial for locating the displaced IUD and guiding appropriate interventions. In cases of significant migration, surgical intervention may be necessary for device retrieval, as you would see in the following case.
A Personal Story
As told to Frontier, a 34-year-old woman had a harrowing experience after she had her IUD treatment. Despite a 17-year-old cesarean scar and IUD insertion 5 years prior, the patient endured four years of intermittent lumbago and abdominal pain. An abdominal wall abscess, rupturing and discharging for 10 days, finally prompted medical attention.
Ultrasound revealed a shocking sight. A V-shaped IUD lodged between the bladder and abdominal wall and adhered to the rectus abdominis muscle through the cesarean scar. CT scans confirmed the device’s precarious position, with one end penetrating the abdominal wall.
A surgical intervention two days later confirmed the migration and facilitated IUD removal. This case starkly illustrates the potential for severe complications from migrated IUDs, even after years of seemingly mild symptoms.
Prevention of Complications
Optimize your Paragard experience through meticulous pre-insertion protocols. Your practitioner should perform a manual examination and sonohysterography to assess uterine morphology. Contraindications include copper hypersensitivity, Wilson’s disease, and uterine anomalies.
Insertion timing is critical. Schedule during days 2-7 of your menstrual cycle to minimize discomfort and ensure non-pregnancy. Your provider will employ tenaculum placement, uterine sounding, and sterile techniques during insertion.
Acquire knowledge about concerning symptoms:
- Excessive menstrual bleeding (>80 mL of blood loss per cycle),
- Severe menstrual pain that does not improve with nonsteroidal anti-inflammatory drugs (NSAIDs),
- Fever without a known cause (>38°C).
Moreover, mastery over the method of transvaginal string palpation can help you conduct monthly self-examinations.
Another non-negotiable for you is to have a stringent follow-up regimen. Initial visit at 4-6 weeks post-insertion, then annually. These appointments should include a pelvic examination, string visualization, and transvaginal ultrasonography to confirm proper IUD positioning.
Your proactive involvement is crucial. Document any unusual symptoms in a menstrual diary. Seek immediate medical attention for acute pelvic pain, amenorrhea, or signs of infection. Your diligence is key to maximizing Paragard’s efficacy and minimizing complications.
FAQs
1. What are the risk factors for uterine perforation with Paragard?
Uterine anomalies like bicornuate or septate uteri increase perforation risk due to atypical anatomy. Immediate postpartum insertion raises the likelihood sevenfold. Insertion during lactation increases the risk by approximately one-third.
2. How soon after Paragard insertion is there a risk of Pelvic Inflammatory Disease (PID)?
According to the Centers for Disease Control and Prevention, the risk of PID from IUDs exists primarily for the first 20 days post-insertion. This underscores the importance of using the aseptic technique during placement.
3. What should I do if I experience complications from Paragard?
If you experience complications, seek immediate medical attention. You may also consider legal action against the manufacturers. Potential Paragard lawsuit settlement amounts are projected to range from $10,000 to $400,000, based on previous similar cases.
This post shows that Paragard’s hormone-free effectiveness comes with potential risks that warrant careful consideration. Understanding these complications empowers users to make informed decisions and take prompt action when necessary.
By staying vigilant, maintaining open communication with healthcare providers, and recognizing early warning signs, users can navigate their contraceptive journey more safely. Remember, your proactive involvement is key to minimizing the risks.